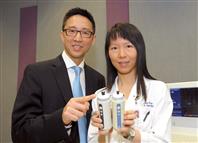
The Chinese University and the University of Bordeaux in France have recently conducted a collaborative research to pioneer the use of the new XL probe to assess liver fibrosis among obese subjects with a deeper penetrance of measurement, and which can also enhance the performance of Fibroscan.
Obesity is closely associated with liver diseases and up to 80% of obese people may have fatty liver, which may lead to cirrhosis and liver cancer. By assessing the severity of liver fibrosis, medical professionals can predict the prognosis of patients and give proper treatment.
Liver biopsy is a traditional standard test to assess liver fibrosis but it is an invasive procedure. Over the last few years, liver stiffness measurement by Fibroscan, an accurate, reproducible and non-invasive test using Doppler ultrasound technique, has been developed to detect liver fibrosis and cirrhosis. But Fibroscan fails to give reliable results in about 30% of obese patients due to their thick subcutaneous fat layer. In view of this, a new XL probe was developed for liver stiffness measurement in obese patients.
From 2009 to 2011, CUHK and the University of Bordeaux conducted a research on liver stiffness measurements on 286 patients by both the new XL probe and the original M probe. Valid measurements were obtained in 98% of patients using the XL probe, compared to 92% when the M probe was in use. Among obese patients with a body mass index above 30 kg/m2, 94% valid measurements were obtained by the XL probe and 74% by the M probe. 































































































































































Social Bookmarks